Unmet needs for medical examination or treatment
In 2022, 4.1 % of the EU population aged 16 years or over had an unmet need for a medical examination or treatment
(%)
Source: Eurostat (hlth_silc_08)
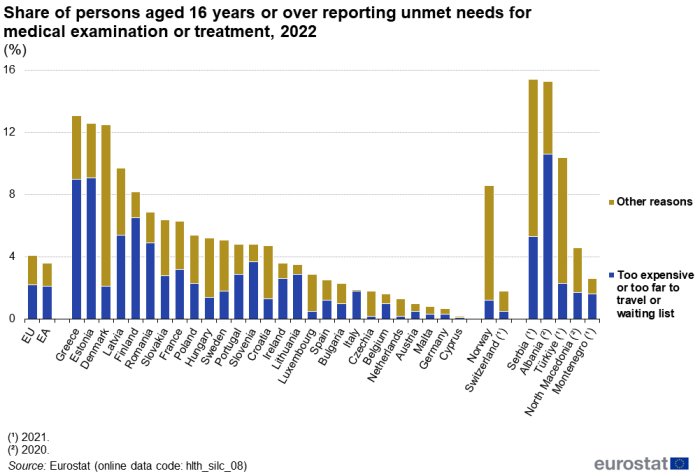
In 2022, 4.1 % of the people aged 16 years or over in the EU reported that they had unmet needs for a medical examination or treatment (hereafter referred to as medical care), a share that ranged from 0.2 % in Cyprus up to 12.5 % in Denmark, 12.6 % in Estonia and 13.1 % in Greece. As regards reasons related to the organisation and functioning of health care services (too expensive, too far to travel or waiting lists), 2.2 % of the EU population reported they had unmet needs, a share that ranged from 0.1 % in Cyprus up to 9.0 % in Greece and 9.1 % in Estonia – see Figure 1.
Being too expensive and waiting lists were the most common main reasons for unmet medical care needs in 2022
(%)
Source: Eurostat (hlth_silc_08)
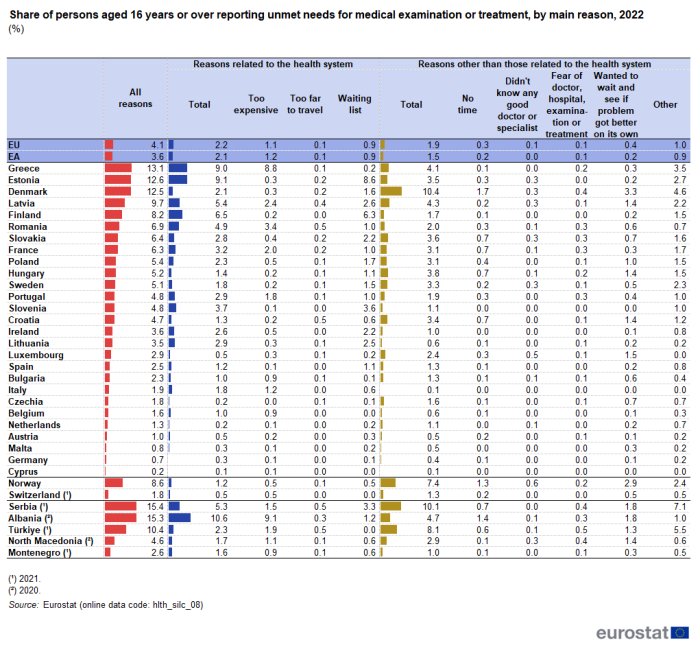
In the EU, the two most common main reasons for unmet needs for medical care in 2022, were that it was too expensive or because of waiting lists. Together these two reasons accounted for almost half of all the people who reported an unmet need for medical care: as a share of the whole survey population, this was 1.1 % for reasons of being too expensive and 0.9 % for waiting lists – see Table 1. The next most common main reasons given were wanting to see if the problem got better on its own (0.4 % of the population) and a lack of time (0.3 % of the population). Less common reasons included fear, not knowing a good doctor or specialist, or that it was too far to travel (all 0.1 %). Aside from the specified main reasons, a further 1.0 % of the population indicated another (unspecified) reason for an unmet need for medical care.
- The expense of medical care was the most frequent specific reason for unmet needs for medical care in Belgium, Bulgaria, Greece, France, Cyprus, Italy, Portugal and Romania, as well as in Montenegro (2021 data), Albania (2020 data) and Türkiye (2021 data). In Germany, as well as in Switzerland (2021 data), the expense of medical care was the joint most frequent reason (along with at least one other specific reason).
- A waiting list hindering medical care was the most frequent specific reason given for unmet needs for medical care in Estonia, Ireland, Spain, Latvia, Lithuania, Austria, Poland, Slovenia, Slovakia, Finland and Sweden in 2022; this was also the case in Serbia (2021 data). In Germany and the Netherlands, a waiting list was the joint most frequent specific reason along with at least one other specific reason.
- Wanting to wait and see if the problem got better on its own was the most frequent specific reason for unmet needs for medical care in Czechia, Denmark, Croatia, Luxembourg, Hungary and Malta; this was also the case in Norway and North Macedonia (2020 data). This was also the joint most frequent specific reason along with at least one other specific reason in Germany and the Netherlands, as well as in Switzerland (2021 data).
EU Member States with a high range – when analysed by age – in the share of people with unmet needs for medical care due to being too expensive, too far to travel or waiting lists displayed relatively high shares for older people
(%)
Source: Eurostat (hlth_silc_08)
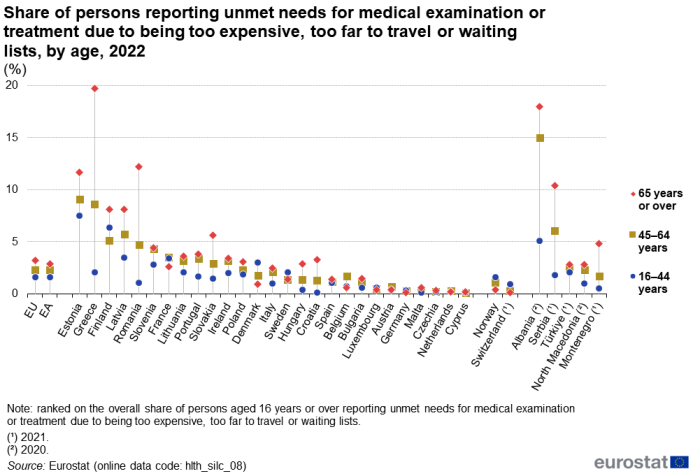
In the EU, 1.6 % of people aged 16–44 years reported unmet needs for medical care in 2022 due to it being too expensive, too far to travel to or because of waiting lists, compared with 2.3 % for people aged 45–64 years and 3.2 % for people aged 65 years or over. In many of the EU Member States, age was a factor linked to unmet needs for medical care due to these reasons, although there was not a universal pattern – see Figure 2.
In general, if EU Member States had a relatively large range – when analysed by age – in the share of people reporting unmet needs for medical care in 2022 due to treatment being too expensive, too far to travel to or because of waiting lists, this was because the share was lowest for younger people and highest for older people. The clearest examples of this pattern were observed in Greece and Romania, where the shares for older people (65 years or over) were 17.6 and 11.1 percentage points, respectively, higher than for the youngest age group (16–44 years). Where the difference between the shares when analysed by age was relatively narrow, the pattern was less clear. In Denmark, the share of people reporting unmet needs for medical care was higher among people aged 16–44 years than it was for people aged 65 years or over (a difference of 2.1 percentage points); this pattern was repeated in France, Sweden, Germany, Luxembourg and Belgium (although the differences were no more than 0.8 percentage points). Within the enlargement countries for which data are presented in Figure 2 (note, mixed reference years), there was a similar pattern to that observed for most of the Member States, with higher shares of older (than younger) people reporting unmet needs for medical care. In Norway and Switzerland (2021 data), a higher share of younger than older people reported unmet needs for medical care.
The share of people reporting unmet needs for medical care for reasons of expense was lowest among people with higher income
(%)
Source: Eurostat (hlth_silc_08)
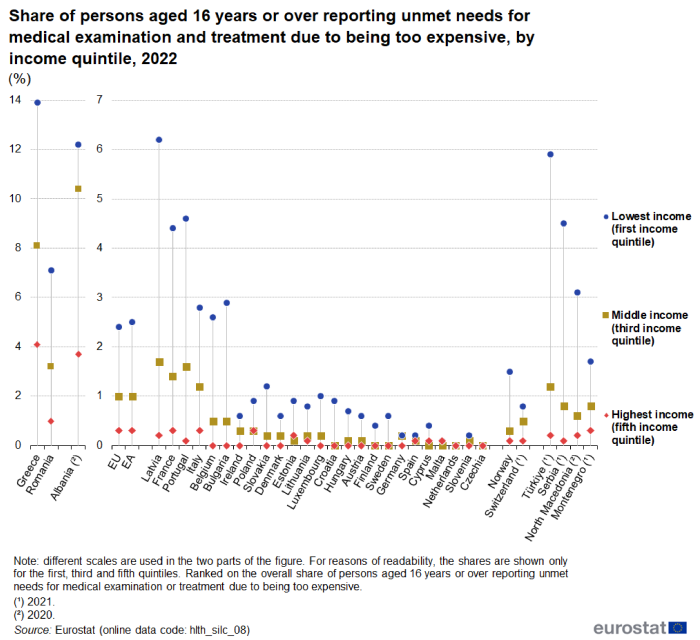
Focusing only on expense, the most common reason for unmet needs for medical care in the EU, and its relation to levels of income, the likelihood of someone reporting an unmet need for this reason was inversely related to their income. In 2022, 2.4 % of the population aged 16 years or over in the first (lowest) income quintile (the 20 % of the population with the lowest income) in the EU reported unmet needs for medical care due to expense, compared with 1.7 % in the second quintile, 1.0 % in the third (middle) quintile, 0.5 % in the fourth quintile and 0.3 % in the fifth (highest) quintile (the 20 % of the population with the highest income).
Figure 3 shows the share of people reporting unmet needs for medical care due to expense and its relation to income: for reasons of readability, the figure shows the shares for the lowest, middle and highest quintiles only. In most of the EU Member States, a similar pattern was observed to that in the EU as a whole: the highest shares of people with unmet needs for medical care due to expense were observed for the first income quintile and the lowest shares for the fifth income quintile, while the shares for the third income quintile lay in between these shares. There were several exceptions in 2022, nearly all of which concerned small differences (0.1 to 0.3 percentage points), often between low shares.
- In Estonia and Cyprus, the shares of people in the middle income quintile with unmet needs for medical care due to expense were lower than the corresponding shares for people in the highest quintile.
- In Spain, Croatia, Poland, Finland and Sweden, the share of people in the middle income quintile with unmet needs for medical care due to expense was the same as the share for people in the highest quintile (and was 0.0 % in both income quintiles for three of these Member States).
- In Malta, the share of people in the middle income quintile with unmet needs for medical care due to expense was lower than the corresponding shares for people in the lowest quintile and the highest quintile.
- In Czechia and the Netherlands, the shares of people with unmet needs for medical care due to expense were 0.0 % for the lowest, middle and highest income quintiles.
The share of people reporting unmet needs for medical care for reasons of expense, too far to travel or waiting lists was lowest for people with higher levels of educational attainment
(%)
Source: Eurostat (hlth_silc_14)
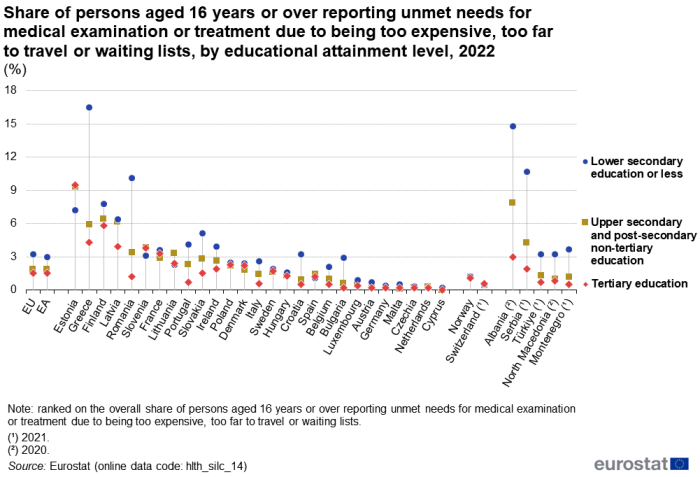
The final analysis for the share of the population reporting unmet needs for medical care due to expense, too far to travel to or waiting lists is based on three groupings showing the highest level of educational attainment – see Figure 4.
In 2022, 1.5 % of people aged 16 years or over in the EU having a tertiary educational attainment reported unmet needs for medical care due to it being too expensive, too far to travel to or because of waiting lists; the corresponding shares were 1.9 % for people having completed upper secondary or post-secondary non-tertiary education and 3.2 % for people having completed, at most, lower secondary education.
- This general pattern of the highest share of people with unmet needs for medical care for the three specified reasons being among people with lower levels of educational attainment (no more than a lower secondary education) was observed in 22 of the EU Member States; this was particularly apparent in Greece and Romania.
- In Spain, Lithuania and the Netherlands, the highest share of people with unmet needs for medical care for the three specified reasons was recorded among people with a medium level of educational attainment (upper secondary and post-secondary non-tertiary education).
- Estonia was the only EU Member State where the reverse situation to that seen for the EU as a whole was observed: the share of people reporting unmet needs for medical care for the three specified reasons was highest for people with higher levels of educational attainment (tertiary education) and lowest for people with lower levels of educational attainment.
- In Slovenia, the highest share of people reporting unmet needs for medical care for the three specified reasons was jointly observed for people with medium or higher levels of educational attainment.
Unmet needs for dental examination and treatment
In 2022, 4.8 % of the EU population had an unmet need for dental examination or treatment
(%)
Source: Eurostat (hlth_silc_22)
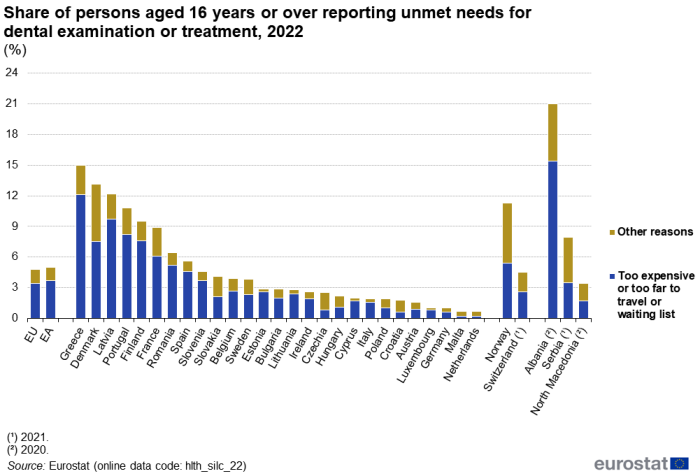
In 2022, 4.8 % of the population aged 16 years or over in the EU reported that they had unmet needs for a dental examination or treatment (hereafter referred to as dental care); as such, the share of the population with unmet needs was slightly greater for dental care than for medical care. The proportion of the population with unmet needs for dental care ranged from 0.7 % in Malta and the Netherlands up to 10.8 % in Portugal, 12.2 % in Lativa and 13.1 % in Denmark, with a peak of 15.0 % in Greece.
If considering only reasons related to the organisation and functioning of health care services – too expensive, too far to travel or waiting lists – 3.4 % of the EU’s population aged 16 years or over reported they had unmet needs. This share ranged from less than 1.0 % in Austria, Czechia, Luxembourg, Germany, Croatia, Malta and the Netherlands up to 9.7 % in Latvia and 12.1 % in Greece – see Figure 5.
Being too expensive was by far the most common main reason for unmet dental care
(%)
Source: Eurostat (hlth_silc_22)
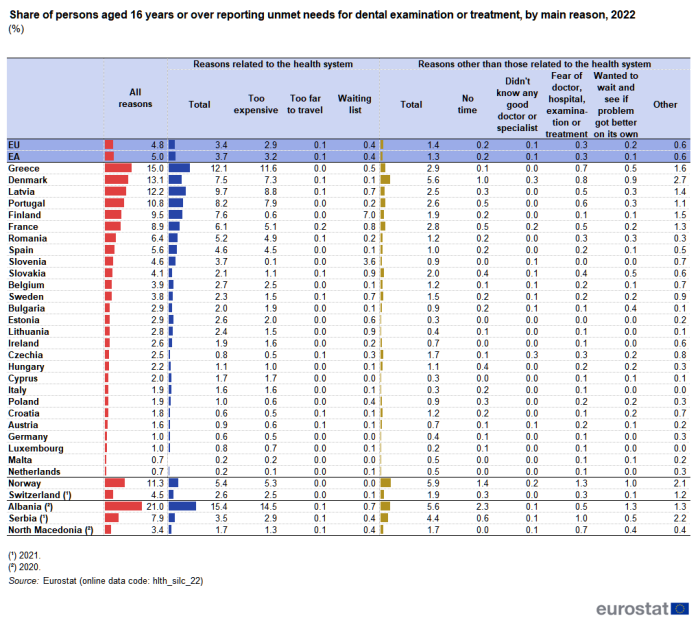
In 2022, the most common main reason for unmet needs for dental care in the EU was being too expensive: 2.9 % of the population aged 16 years or over reported unmet needs for this main reason, which was approximately three fifths of all reasons – see Table 2. After expense, the next most common reasons reported for unmet needs for dental care were waiting lists (0.4 % of the population) or fear (0.3 %). Less common reasons included a lack of time or wanting to wait and see if the problem got better on its own (both 0.2 %) or that it was too far to travel or the respondent did not know a good doctor or specialist (both 0.1 %). Aside from the specified main reasons, 0.6 % of the population indicated another (unspecified) reason for an unmet need for dental care.
The expense of dental care was the most common specific reason for unmet needs for dental care in 24 EU Member States; it was also the most frequent reason in all of the non-EU countries shown in Table 2 (note there are various reference years). In Cyprus, Italy, Spain, Greece and Romania, more than three quarters of all people with an unmet need for dental care said that the main reason was because of expense.
There were only three exceptions among the EU Member States where expense was not the main reason for unmet needs for dental care in 2022. A waiting list hindering dental care was the most common specific reason given for unmet needs for dental care in Finland and Slovenia. Approximately three quarters of the people with an unmet need for dental care in these two EU Member States reported that the main reason was because of waiting lists. In the Netherlands, a very low share of people reported unmet needs for dental care, with equal shares for expense, waiting lists and fear (all 0.1 %).
Unmet needs for dental care due to expense, too far to travel or waiting lists were most often reported by people aged 45–64 years
(%)
Source: Eurostat (hlth_silc_22)
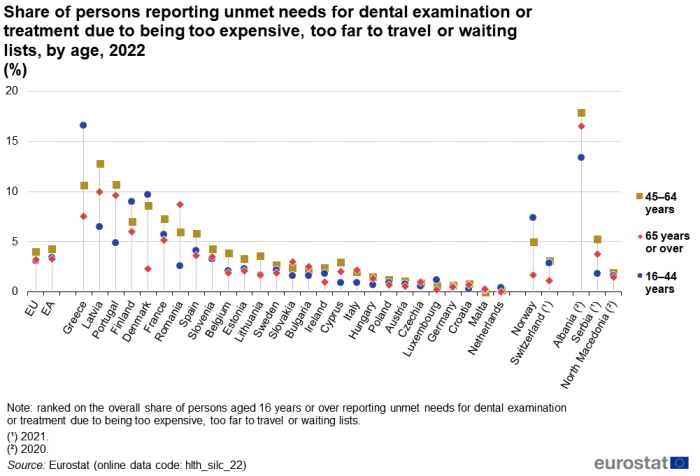
In the EU, 4.0 % of persons aged 45–64 years reported unmet needs for dental care due to expense, too far to travel or waiting lists in 2022. This was higher than the corresponding shares for younger people (3.1 %; aged 16–44 years) or older people (3.2 %; 65 years or over) – see Figure 6.
- In 16 EU Member States, people aged 45–64 years were most likely to report unmet needs for dental care due to expense, too far to travel or waiting lists; this was also the case in Switzerland (2021 data) as well as North Macedonia (2020 data), Albania (2020 data) and Serbia (2021 data).
- In Bulgaria, Czechia, Italy, Malta, Romania and Slovakia, people in the oldest age group (aged 65 years or over) were most likely to report unmet needs for dental care due to expense, too far to travel or waiting lists; in all of these Member States except Malta, the share was lowest for people aged 16–44 years.
- In Denmark, Greece, Luxembourg, the Netherlands and Finland, people in the youngest age group (aged 16–44 years) were most likely to report unmet needs for dental care due to expense, too far to travel or waiting lists; in all five of these Member States, the share was highest for people aged 16–44 years and lowest for people aged 65 years or over; this was also the case in Norway.
Source data for tables and graphs
Data sources
The data used in this article are derived from EU statistics on income and living conditions (EU-SILC). This source provides annual data for the EU Member States as well as most EFTA and enlargement countries on income, poverty, social exclusion and other aspects of living conditions.
The reference population for EU-SILC is limited to private households and their current members residing in the territory of the surveying country at the time of data collection. People living in collective households and institutions are generally excluded from the reference population. All household members are surveyed, but only those aged 16 years or over are interviewed.
Questions included in EU-SILC on medical and dental examination or treatment refer to a person’s own assessment of whether they needed examination or treatment for the specific types of health care (medical and dental) in the previous 12 months but did not have it or did not seek it.
The source is documented in more detail in this background article which provides information on the scope of the data, its legal basis, the methodology employed, as well as related concepts and definitions.
Limitations of the data
All of the indicators presented in this article are derived from self-reported data so they are, to a certain extent, affected by respondents’ subjective perception as well as by their social and cultural background. Despite their subjective nature, the statistics that are presented are considered to be relevant and reliable estimators of the health status of populations as well as good predictors of health care needs; they are also valuable for trend analyses and for measuring socioeconomic disparities.
EU-SILC does not cover the institutionalised population, for example, people living in health and social care institutions whose health status is likely to be worse than that of the population living in private households. It is therefore likely that, to some degree, this data source under-estimates the share of the population with health problems. By contrast, the exclusion of health and social care institutions, where medical care is likely to be readily available, may lead to an over-estimation of unmet needs for health care.
Another factor that may influence the results shown is the different organisation of health care services, be that nationally or locally. Furthermore, the indicators presented are not age-standardised and thus reflect the current national age structures. Finally, despite substantial and continuous efforts for harmonisation, the implementation of EU-SILC is organised nationally, which may impact on the results presented, for example, due to differences in the formulation of questions or their precise coverage.
Context
Good health is an asset in itself. It is not only of value to the individual as a major determinant of quality of life, well-being and social participation, but it also contributes to general social and economic growth. Many factors influence the health status of a population, and these can be addressed by health and other policies regionally, nationally or across the EU.
Barriers to accessing health care include cost, distance, waiting times, lack of cultural sensitivities and discrimination. For non-native speakers, language can be an obstacle for those seeking to access services, while barriers to health care may also result from poor understanding or a lack of knowledge with respect to a patient’s rights and the administrative practices and requirements of health systems.
A European Commission Communication Towards social investment for growth and cohesion (COM(2013) 83 final) and its accompanying document on Investing in health (SWD(2013) 43) highlight the need to invest in sustainable health systems which can improve cohesion and boost economic growth by reducing health inequalities, enabling people to remain active longer and in better health. The EU4Health programme 2021–2027 – a vision for a healthier European Union sets out four general objectives:
- improving and fostering health;
- protecting people;
- access to medicinal products, medical devices and crisis-relevant products (ensuring that these products are accessible, available and affordable);
- strengthening health systems.
Investment designed to reduce health inequalities should contribute to increased social cohesion and may help break the spiral of poor health that both contributes to and results from poverty and exclusion. Health inequalities represent a considerable burden both in terms of their effect on an individual’s health, as well as productivity losses and costs associated with social protection systems.
An indicator on the equality of access to health care service, defined as the total self-reported unmet need for medical care for the reasons of financial barriers, waiting times and too far to travel, is included in the health services chapter of the European core health indicators (ECHI).